Book Appointment Now
Free Pediatric Dose Calculator
Pediatric Dose by Weight Calculator
The Pediatric Dose by Weight Calculator is a valuable tool for determining the appropriate medication dosage for children based on their weight. This method is commonly used because it ensures the dose is tailored to the individual child's body mass, providing a more accurate and safe dosage.
How to Use:
- Weight: Enter the child's weight in either kilograms (kg) or pounds (lbs).
- Dosage: Enter the prescribed dosage in mg/kg or mcg/kg.
- Frequency: Select how often the medication should be administered (e.g., once a day, twice a day).
- Click "Calculate Dose" to see the appropriate dose per administration.
Pediatric Dose by BSA Calculator
The Pediatric Dose by BSA Calculator is designed to determine medication dosages based on a child's Body Surface Area (BSA). BSA is a more precise measurement for dosing certain medications, especially chemotherapy and other potent drugs.
How to Use:
- Weight: Enter the child's weight in either kilograms (kg) or pounds (lbs).
- Height: Enter the child's height in either centimeters (cm) or inches.
- Dosage: Enter the prescribed dosage in mg/m² or mcg/m².
- Frequency: Select how often the medication should be administered.
- Click "Calculate Dose" to see the appropriate dose per administration.
This method is particularly beneficial for calculating dosages of medications where precise dosing is critical to efficacy and safety.
Pediatric Dose by Young's Rule Calculator
Young's Rule is a simple and widely used method for calculating pediatric medication doses based on the child's age. This method is particularly useful for general medications where age-based dosing is appropriate.
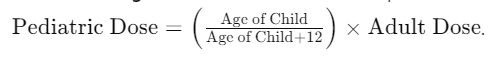
How to Use:
- Age: Enter the child's age in years.
- Adult Dose: Enter the adult dose in either mg/day or mcg/day.
- Frequency: Select how often the medication should be administered.
- Click "Calculate Dose" to see the appropriate dose per administration.
Young's Rule helps to adapt the adult dose to a pediatric patient by considering the child's age, ensuring a safer dosage.
Pediatric Dose by Clark's Rule Calculator
Clark's Rule is another method used to calculate the pediatric medication dose based on the child's weight. The formula is:
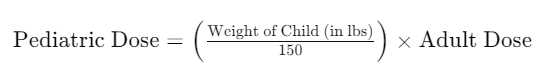
This method is straightforward and effective for adjusting adult doses to suit pediatric patients.
How to Use:
- Weight: Enter the child's weight in pounds (lbs).
- Adult Dose: Enter the adult dose in either mg/day, mg/dose, mcg/day, or mcg/dose.
- Frequency: Select how often the medication should be administered.
- Click "Calculate Dose" to see the appropriate dose per administration.
Clark's Rule is instrumental when the child's weight is known and provides a quick way to calculate a safe dose.
Understanding Pediatric Dosage
Administering the correct medication dosage to children is crucial to ensure their safety and efficacy. Unlike adults, children require specially calculated doses based on various factors such as weight, body surface area (BSA), age, and specific physiological conditions.
Pediatric dosage calculations aim to tailor the medication to the child's specific needs, preventing underdosing or overdosing, both of which can lead to serious health consequences.
Importance of Accurate Pediatric Dosing
- Safety: Accurate dosing prevents adverse drug reactions and toxicity, which can occur if a child is given too much medication.
- Efficacy: Ensuring the correct dose means the medication will effectively treat the condition, helping the child recover faster.
- Developmental Considerations: Children's metabolic rates and organ functions differ from adults, and their bodies process medications differently. Accurate dosing takes these factors into account.
- Compliance: Accurate dosage calculations can help design more palatable medication regimens, increasing the likelihood that children will comply with their medication schedules.
Factors Affecting Pediatric Dosage
- Age: Children of different ages metabolize drugs at different rates. Age can influence the required dosage and frequency of administration.
- Weight: Heavier children typically require larger doses than lighter children.
- BSA: This accounts for both weight and height, providing a more precise dosage for certain medications.
- Health Conditions: Pre-existing health conditions like kidney or liver disease can affect how medications are processed and may require dose adjustments.
- Pharmacokinetics and Pharmacodynamics: These principles describe how the drug moves through the body (absorption, distribution, metabolism, and excretion) and how it affects the body, respectively.
Dosage Adjustment Factors
While the standard pediatric dosage calculation methods provide a good starting point, various factors may necessitate adjustments to the calculated dose. These adjustments are crucial to ensure the safety and efficacy of the medication for each individual patient.
Here are some common factors that may require dosage adjustments:
- Renal Impairment: Many drugs are excreted through the kidneys, and impaired renal function can lead to drug accumulation and potential toxicity. In such cases, the dosage may need to be reduced or the dosing interval extended to prevent adverse effects. Dosage adjustments may be based on the patient's estimated glomerular filtration rate (eGFR) or other measures of renal function.
- Hepatic Impairment: The liver plays a vital role in drug metabolism, and impaired liver function can affect the way drugs are metabolized and eliminated from the body. Patients with hepatic impairment may require lower doses or longer dosing intervals to prevent drug accumulation and potential toxicity.
- Drug Interactions: Certain medications can interact with other drugs, altering their pharmacokinetics (absorption, distribution, metabolism, or excretion) or pharmacodynamics (therapeutic effects). These interactions may necessitate dosage adjustments to maintain the desired therapeutic effect or prevent adverse reactions.
- Genetic Factors: Genetic variations can influence how an individual metabolizes or responds to certain medications. For example, some patients may be poor or rapid metabolizers of specific drugs, which can affect the drug's efficacy or toxicity. In such cases, dosage adjustments may be necessary based on the patient's genetic profile.
- Age and Developmental Stage: Pediatric patients undergo various developmental changes as they grow, affecting drug metabolism and response. Dosage adjustments may be required based on the child's age, weight, and developmental stage to ensure appropriate drug exposure and minimize adverse effects.
- Concomitant Illnesses or Conditions: Certain medical conditions, such as cardiovascular disease, respiratory disorders, or cancer, can alter the pharmacokinetics or pharmacodynamics of medications. Dosage adjustments may be necessary to account for these conditions and ensure safe and effective treatment.
- Therapeutic Drug Monitoring (TDM): For certain medications with a narrow therapeutic index (the range between effective and toxic concentrations), therapeutic drug monitoring may be employed to measure the drug levels in the patient's blood. Based on the measured drug concentrations, dosage adjustments can then be made to maintain levels within the therapeutic range.
Medication Administration Frequencies Explained
The frequency at which medication is administered is a crucial aspect of treatment plans, ensuring that the drug maintains its efficacy and safety throughout the course of therapy. Different frequencies are prescribed based on the medication's pharmacokinetics (how the drug is absorbed, distributed, metabolized, and excreted) and pharmacodynamics (the drug's effects on the body).
Common Administration Frequencies
Here's a detailed explanation of common medication administration frequencies used in pediatric and adult treatments:
- qD (quaque die) - Once a Day: Medications are taken once every 24 hours. This frequency is convenient and is often used for medications with a long half-life or formulated to release slowly over time.
- BID (bis in die) - Twice a Day: Medications are taken every 12 hours. This frequency helps maintain stable drug levels in the body, often used for antibiotics and other medications that require more consistent blood levels.
- TID (ter in die) - Three Times a Day: Medications are taken every 8 hours. This frequency ensures that the medication is present in the body throughout the day and night, which is suitable for drugs with shorter half-lives.
- QID (quater in die) - Four Times a Day: Medications are taken every 6 hours. This frequent dosing is typically used for medications that are rapidly metabolized and excreted.
- q8h (quaque 8 hora) - Every 8 Hours: Medications are taken every 8 hours. Like TID, this ensures around-the-clock medication levels but specifically refers to an 8-hour interval.
- q6h (quaque 6 hora) - Every 6 Hours: Medications are taken every 6 hours, ensuring frequent dosing for drugs that require steady levels in the bloodstream.
- q4h (quaque 4 hora) - Every 4 Hours: Medications are taken every 4 hours. This frequency is less common and usually reserved for specific conditions requiring constant drug levels.
- q3h (quaque 3 hora) - Every 3 Hours: Medications are taken every 3 hours. Used rarely, typically in acute care settings.
- q2h (quaque 2 hora) - Every 2 Hours: Medications are taken every 2 hours. This is usually used in critical care for drugs that need to be maintained at a very steady level.
- q1h (quaque 1 hora) - Every Hour: Medications are taken every hour. This frequency is very rare and usually applicable in intensive care situations.
Table of Administration Frequencies
| Frequency | Abbreviation | Latin Term | Interval |
|---|---|---|---|
| Once a day | qD | quaque die | Every 24 hours |
| Twice a day | BID | bis in die | Every 12 hours |
| Three times a day | TID | ter in die | Every 8 hours |
| Four times a day | QID | quater in die | Every 6 hours |
| Every 8 hours | q8h | quaque 8 hora | Every 8 hours |
| Every 6 hours | q6h | quaque 6 hora | Every 6 hours |
| Every 4 hours | q4h | quaque 4 hora | Every 4 hours |
| Every 3 hours | q3h | quaque 3 hora | Every 3 hours |
| Every 2 hours | q2h | quaque 2 hora | Every 2 hours |
| Every hour | q1h | quaque 1 hora | Every hour |
Importance of Adhering to Administration Frequencies
- Therapeutic Effectiveness: Properly spaced doses ensure that medication levels in the body remain within the therapeutic range, enhancing efficacy.
- Safety: Avoiding overdose or underdose by adhering to prescribed frequencies helps prevent adverse effects and treatment failures.
- Convenience: Some regimens are designed for convenience to improve patient adherence, especially for chronic conditions.
- Steady-State Concentration: Certain medications require steady levels in the bloodstream to work effectively, which can only be achieved through proper dosing intervals.
Understanding and following the prescribed medication administration frequencies is vital for the success of any treatment plan. It ensures that the medication works effectively, maintains its therapeutic effect, and minimizes the risk of side effects.
Always consult with healthcare professionals for any questions or concerns about medication schedules.
Common Administration Frequencies
Proper medication administration is essential to ensure the safety and effectiveness of treatment, particularly in pediatric patients. Different routes of administration and dosage forms require specific techniques to ensure accurate dosing and minimize the risk of adverse effects. Here are some important considerations and techniques for administering medications to pediatric patients:
- Oral Administration
- Tablets/Capsules: For children who cannot swallow whole tablets or capsules, crushing or opening the dosage form and mixing it with a small amount of soft food or liquid may be necessary. However, certain medications should not be crushed or opened due to their formulation or properties.
- Liquids: Pediatric patients often prefer oral liquids, such as suspensions or syrups. Measure the precise dose using a calibrated oral syringe or medication cup. Shake the liquid well before measuring if instructed.
- Flavoring agents: Some medications have an unpleasant taste, making administration challenging. Flavoring agents like juice, honey, or sweeteners may help improve palatability and increase adherence.
- Intravenous (IV) Administration
- Verify the correct IV line and ensure proper patency and flushing.
- Calculate the dose based on the concentration of the IV solution and the patient's weight or body surface area.
- Use an infusion pump or IV drip set to control the rate of administration and ensure accurate dosing.
- Monitor for potential adverse reactions, such as extravasation or infiltration.
- Intramuscular (IM) and Subcutaneous (SC) Injections
- Select the appropriate needle size and length based on the patient's age, weight, and injection site.
- Use proper landmarks and injection techniques (e.g., Z-track method for IM injections) to minimize discomfort and ensure accurate delivery.
- Rotate injection sites to prevent tissue damage and discomfort.
- Aspiration before injection is recommended for IM injections to ensure the needle is not in a blood vessel.
- Inhalation Administration
- Use age-appropriate devices, such as nebulizers or metered-dose inhalers (MDIs) with spacers or valved holding chambers.
- Provide proper instructions and demonstrations on device usage and breathing techniques to ensure optimal drug delivery.
- Monitor for potential side effects, such as bronchospasm or paradoxical reactions.
- Topical Administration
- Ensure proper skin preparation and cleansing before applying topical medications.
- Use appropriate applicators or gloves to avoid contamination and ensure accurate dosing.
- Educate caregivers on the correct application techniques and precautions (e.g., avoiding occlusion, sun exposure).
- General Considerations
- Always double-check the medication, dosage, route, and patient information before administration.
- Involve caregivers and pediatric patients (when appropriate) in the administration process to promote adherence and understanding.
- Monitor for potential adverse effects, drug interactions, and therapeutic responses.
- Document all medication administrations wholly and accurately.
References
Books and Articles
- "Pediatric Dosage Handbook" by Carol K. Taketomo, Jane H. Hodding, and Donna M. Kraus
- This comprehensive handbook provides detailed information on the dosing of medications for pediatric patients, including weight-based, BSA-based, and age-based dosing methods.
- "The Harriet Lane Handbook: A Manual for Pediatric House Officers" by Johns Hopkins Hospital
- A practical manual includes guidelines on pediatric dosages, medication administration, and treatment protocols.
- "Clinical Pharmacokinetics and Pharmacodynamics: Concepts and Applications" by Malcolm Rowland and Thomas N. Tozer
- This book offers an in-depth knowledge of pharmacokinetics and pharmacodynamics, essential for understanding how drugs behave in the pediatric population.
Online Resources
- MedlinePlus - Pediatric Medication:
- MedlinePlus - Pediatric Medication
- A resource from the National Library of Medicine that provides information on pediatric medications, including dosages and safety tips.
- American Academy of Pediatrics (AAP):
- American Academy of Pediatrics
- The AAP provides guidelines, research, and recommendations on pediatric healthcare, including medication dosages.
- World Health Organization (WHO) - Pediatric Pharmacology:
- WHO - Pediatric Pharmacology
- The WHO offers guidelines and resources on pediatric pharmacology and safe medication practices for children.
Clinical Guidelines
- Pediatric Pharmacotherapy: A Guide for the Non-Pediatric Practitioner:
- Provides guidelines and principles for safe and effective medication use in children.
- National Institute for Health and Care Excellence (NICE) - Medicines Optimisation:
- NICE - Medicines Optimisation
- Offers guidelines on optimizing the use of medications, including pediatric dosing recommendations.